A woman and her children walk past a sign for a U.S. Agency for International Development program in Dikwa, Nigeria, April 29, 2025. (AP/Sunday Alamba)
Relief organizations and others have been sounding the alarm on the human toll from the Trump administration's pullback in humanitarian aid funding, which has affected a range of work around the world and has ultimately resulted in deaths.
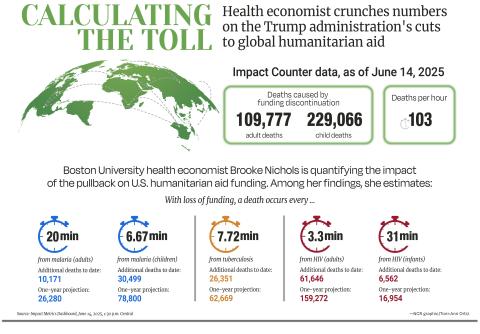
One of the people raising concerns is Brooke Nichols, a Boston University associate professor of global health who models infectious diseases and used to work on a program funded by the U.S. Agency for International Development herself. In light of the funding cuts, Nichols, a health economist, started crunching the numbers to quantify the impact.
Those calculations can now be found on a website called the Impact Counter, where the data is broken down into different categories, like HIV prevention and tuberculosis treatment.
As of June 15, the death toll for adults and children from aid funding cuts topped 340,000 and came out to 103 deaths per hour.
National Catholic Reporter talked to Nichols over the phone about how the modeling works, its accuracy, what drew her to this project and what some critics have said. NCR edited the interview for conciseness and clarity.
NCR: Can you explain how you calculate the lives that have been lost from the cutting of aid? Is this really tough to do mathematically, or easier than we might think?
Nichols: There's a lot of different numbers on the counter now. So there is for TB, HIV, malaria, also pneumonia, malnutrition, diarrhea, and each of those are different and calculated in [a] slightly different way, but the core principles are the same.
We know, let's say, what the mortality rate is of these different diseases if we do an intervention or if we don't do an intervention. And roughly, if you know how many people were receiving the intervention — so whatever it might be, if it's treatment or vaccines — then we know how many people were accessing that through USAID-funded line items. Then you can figure out the difference in mortality with and without it. So it's really quite simple in a way.
It's relatively simple for things like diarrhea, pneumonia and malnutrition, because it's sort of mortality rate with and without and the total number of people. But HIV, malaria, TB, infectious diseases — there are more sophisticated mathematical models that really try to estimate also the onward consequences of some of this, like increased transmission that could result in additional mortality and those types of things. So those are [a] bit more complicated, but the principle I think ultimately is the same.
What's the margin for error in the calculations? How big of a grain of salt should we take with them?
I think the error bars at present are wide. I don't think that these are precise estimates by any stretch of the imagination, for two reasons.
One is we don't know the extent to which countries, organizations, individuals have stepped up to fill the gaps. There's no systematic reckoning of how people have been dealing with this and this loss of funding. That could be a lot of gap-filling that's already been done or not. So that's a major source of uncertainty.
And then the other thing is that some of these things take time. So we've calculated a full year of impact. So if you had this intervention over the course of the year, or you didn't, how many people would die, and then just drew sort of a straight line to then count.

In Sarmada district, Syria, on Feb. 9, 2025, Dr. Mohammad Fares shows an empty pharmacy at the Sarmada Health Center, which was closed due to the suspension of U.S. support for several organizations in northwestern Syria. (AP/Ghaith Alsayed)
But in reality, there's different amounts of stockpiles of drugs that might be available, and so we might not start to see the effects until a few months in, and they might start slowly and then grow exponentially. So I think the numbers reflect if there were that gap of funding, and that gap of funding was not filled, that's how many people would die.
So it can't account for the gray as much as it's black and white, but still kind of gives you something to go off of theoretically?
Yeah, exactly. There's ways in which we maybe overestimate death. But I think there's things we're not measuring that would go the other direction. We calculate these sort of direct effects, but not the effects on the broader health care systems which could be affected.
So if you're pulling personnel from your outpatient department or your hospital to staff your HIV clinic, because there's no staff, that could negatively affect health outcomes for people going to the clinic because they broke their arm. We don't really capture these types of effects as well.
How long does it take, by your estimate, from the time money like this is cut to when we actually see impacts and increased illness or death on the ground?
I think it's different for each different disease. I think in terms of stockpiles, people usually have three months of supplies on hand. So that's when you'd start to see it. Not from day one. But for some things like malnutrition, that could happen from as early as day one. Food supplies don't last for three months. They last typically much less time.
Some of these, they're complicated and interdependent and each country will respond in a different way. So I think some countries will see impact sooner than others, just sort of depending on how much they rely on PEPFAR for funding, let's say, or USAID funding.

A worker with Catholic Relief Services assists a mother with her baby for a nutrition screening in Port-au-Prince, Haiti, July 20, 2020. (OSV News/Catholic Relief Services)
Would there be a way to calculate at all the deaths caused by funding cuts to a specific organization like Catholic Relief Services by itself, just because they're such a big recipient of government funds? Or would you have to add up individually from individual programs and then kind of look at the funding proportion?
[I'd] kind of have to see what CRS funds. Like, what are the different programs that they fund, and how many people do they deliver services to and what are the services and then you could calculate their relative impact of being cut.
What compelled you to start this project?
I used to work and live in South Africa for three years, and I worked a lot in other neighboring countries as well on a USAID-funded project. A lot of my work still is with people in that region and on similar topics.
I was on those projects to make them efficient. I was a health economist trying to figure out how to do the most cost-effective things, to find more people, make sure that they stay healthy, and so I know just how efficient those programs were. I've never worked with a donor that's that focused on hitting their indicators and improving their outcomes.
So to hear it called wasteful and fraud and all of that, just like, what? It's unimaginable to me. It was a program that really tried to succeed. It really tried to be efficient and not wasteful.
Advertisement
I'm surprised how many pastors and reverends and various people have reached out in a really kind way, wanting to help. People that they provide services to that are part of their congregations, that they really care, that they're moved by the moral argument of providing aid. These are people from the middle of the country.
I was just shocked.
When people reach out and ask how can they help, what do you tell them?
They seem to want to help to show the impact, or they want to talk about what it means, or I've been sort of asked to talk to different groups, like congregations, about what this means. I had one reach out that really wants to go and document the impact and help elevate this work in a different way and using his networks through different countries.
People, they want to do something about it. And I'm glad a lot of people find that this is unacceptable and want to show that to people.
And I think the numbers are not compelling to most people. Numbers are numbers. What's compelling are people and stories. And I'm so appreciative of the people that do that work and show what the impacts look like on an individual, personal level.
I have a feeling for what these numbers mean. I imagine that, [for] most people, that's a number.
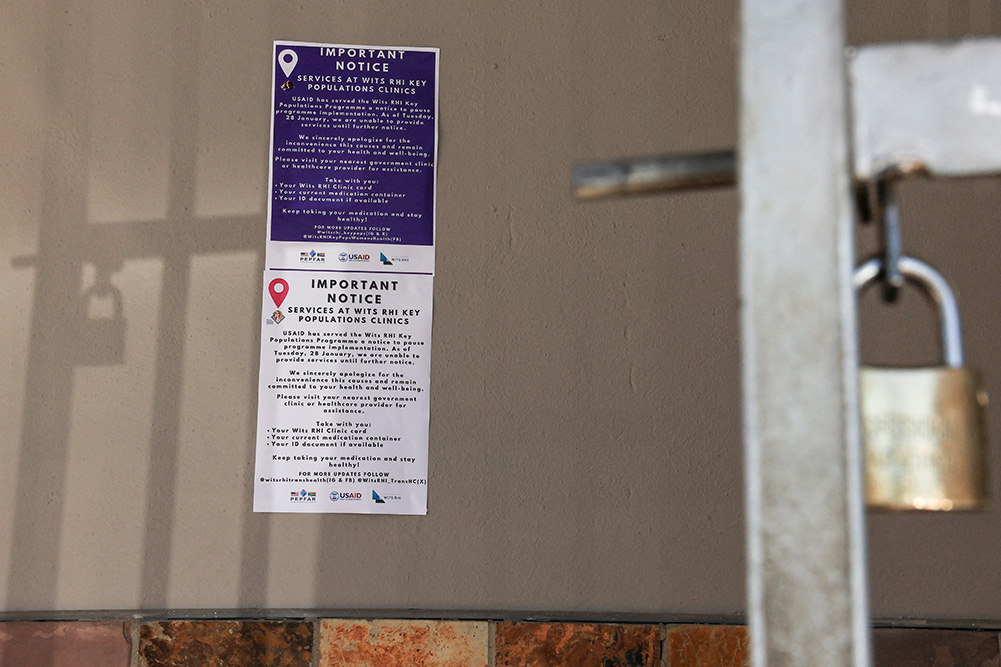
A notice outside a clinic Jan. 28, 2025, states that Wits RHI Key Population Program in Cape Town, South Africa, is unable to provide services until further notice following a USAID notification to pause the program. (OSV News/Reuters/Esa Alexander)
Whereas, if you hear an anecdote you're saying, it kind of pulls at your heartstrings a little bit more.
Exactly. Another piece of feedback has been, well, where are the body bags? ... A lot of people are like, well, if this many people have died, where's the body bags?
And what people might fail to realize with this is these are causes of death, things that kill people anyway. A change in mortality rate of things that people were already dying from. If I look at it across a whole continent, it would be worse comes to worse, up to a 10% increase in mortality. But if you are in a village, and let's say 10 people die a year, and now 11 people die this year, would you notice?
I would wonder, too, is when someone [dies] is that formalized?
These systems don't exist in many places to do mortality studies. The United States is pretty special, parts of Europe as well. But we have that CDC WONDER tool where we can see how everyone in the United States has died in the last however many years. That doesn't exist in most countries.
And also just the effects are so spread across different countries and regions that you just wouldn't notice.
Are estimates like this kind of the best that we'll ultimately be able to get to determine the overall impact?
Probably.